A new scoping review published in the European Journal of Pediatrics has shed light on the health challenges faced by children with profound intellectual and multiple disabilities (PIMD). The study, conducted by researchers from Radboud University Medical Centre in the Netherlands, highlights the most prevalent health problems in this vulnerable population, including epilepsy, respiratory infections, feeding difficulties, gastroesophageal reflux disease (GERD), scoliosis, and visual impairment. The findings underscore the urgent need for more research and better care coordination for children with PIMD.
What is PIMD?
Profound intellectual and multiple disabilities (PIMD) refer to a combination of severe intellectual disability (IQ or developmental quotient < 35) and profound motor impairment, often classified as Gross Motor Function Classification System (GMFCS) level IV or V. Children with PIMD are non-ambulatory and require intensive support for daily living. They also frequently experience sensory impairments and a range of comorbidities, making their care complex and multifaceted.
Despite the significant health challenges faced by children with PIMD, there is a lack of uniformity in the definition and terminology used to describe this population. This has led to fragmented care and limited research on their specific health needs.
Key Findings of the Study
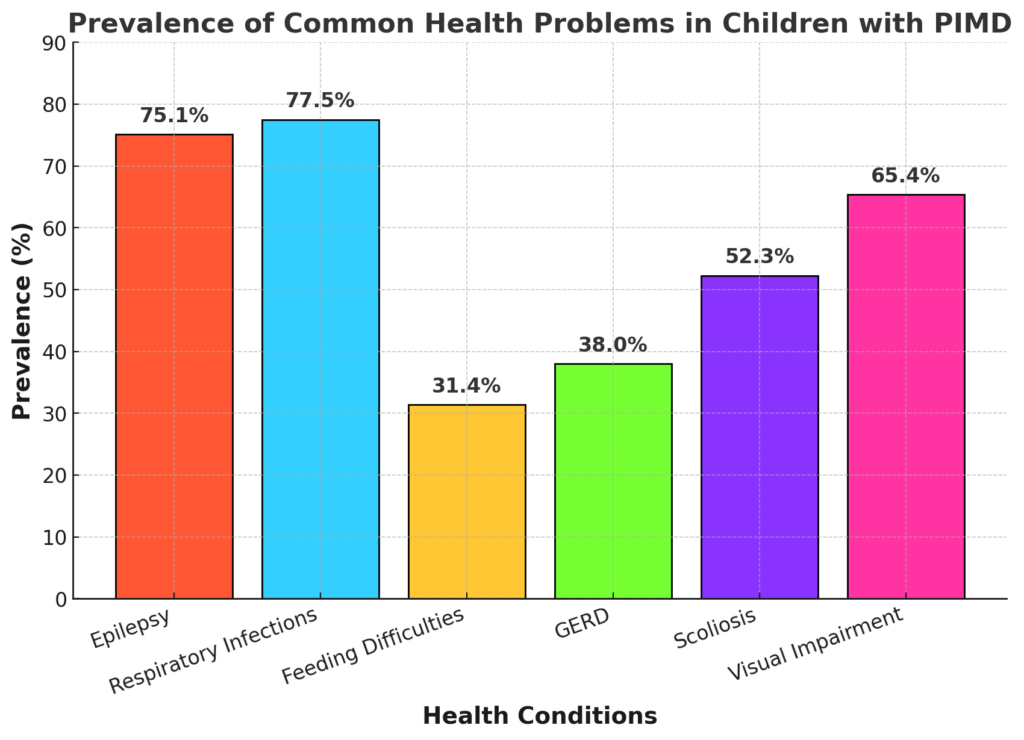
The scoping review, which analyzed 22 studies involving 894 children with PIMD, identified the following as the most common health problems:
Visual Impairment: Nearly 65% of children had some form of visual impairment, further complicating their care and quality of life.
Epilepsy: Nearly 75% of children with PIMD were reported to have epilepsy, making it the most prevalent health issue.
Respiratory Infections: Over 77% of children experienced respiratory infections, often due to aspiration or other complications.
Feeding Difficulties: Approximately 31% of children had feeding difficulties, including problems with swallowing and the need for feeding tubes.
GERD: Gastroesophageal reflux disease (GERD) was reported in 38% of children, leading to discomfort and further complications.
Scoliosis: About 42% of children had scoliosis, a condition that can exacerbate respiratory and mobility issues.
The Burden on Families and Caregivers
Children with PIMD often require frequent hospital visits and complex, multidisciplinary care. This places a significant emotional and financial burden on their families. According to the study, parents of children with PIMD often struggle with the strain of managing frequent medical appointments, arranging transportation, and providing care for other siblings. The financial impact can be substantial, as parents may need to take time off work or incur additional expenses for specialized care.
The study also highlights the fragmented nature of care for children with PIMD. With multiple medical specialists involved, including pediatricians, rehabilitation physicians, physiotherapists, and speech therapists, it is often unclear who is responsible for coordinating the child’s care. This lack of coordination can lead to gaps in treatment and unmet health needs.
The Need for Early Detection and Proactive Care
One of the key takeaways from the study is the importance of early detection and proactive care for children with PIMD. Undiagnosed and untreated health problems can lead to the development of secondary complications, further reducing the child’s quality of life. For example, untreated GERD can lead to chronic respiratory issues, while unmanaged epilepsy can result in developmental delays and behavioral problems.
The researchers emphasize the need for regular health screenings and a comprehensive approach to care. Early intervention can help prevent unscheduled hospital visits and improve long-term outcomes for children with PIMD.
Challenges in Research and Terminology
The study also highlights the challenges in conducting research on children with PIMD. The lack of a uniform definition and terminology for PIMD has made it difficult to compare findings across studies and develop standardized care protocols. The researchers call for a consensus definition of PIMD to improve the accessibility and quality of research in this field.
Additionally, the study found that there is limited information on the age of onset for various health problems and the effectiveness of treatments. This gap in knowledge makes it challenging to develop targeted interventions and care plans for children with PIMD.
Future Research Directions
The researchers recommend further studies to explore the age of onset for health problems in children with PIMD and to evaluate the effectiveness of various treatments. They also suggest that future research should include behavioral and psychological health problems, which were not the focus of this review but are known to significantly impact the quality of life for children with PIMD and their families.
The ultimate goal of this research is to develop a multidisciplinary care pathway that ensures children with PIMD receive timely and appropriate care. By creating a “patient journey” that outlines the roles of different healthcare professionals, the researchers hope to improve care coordination and outcomes for this vulnerable population.
Conclusion
This scoping review provides valuable insights into the health challenges faced by children with profound intellectual and multiple disabilities. The most common health problems include epilepsy, respiratory infections, feeding difficulties, GERD, scoliosis, and visual impairment. However, the lack of a uniform definition and limited research on treatment options highlight the need for further studies in this area.
Early detection and proactive care are essential to improving the quality of life for children with PIMD. By addressing these health problems early and coordinating care more effectively, healthcare providers can help reduce the burden on families and improve outcomes for children with PIMD

